Patients immersed in VR could need less anaesthetic during surgery, new study finds
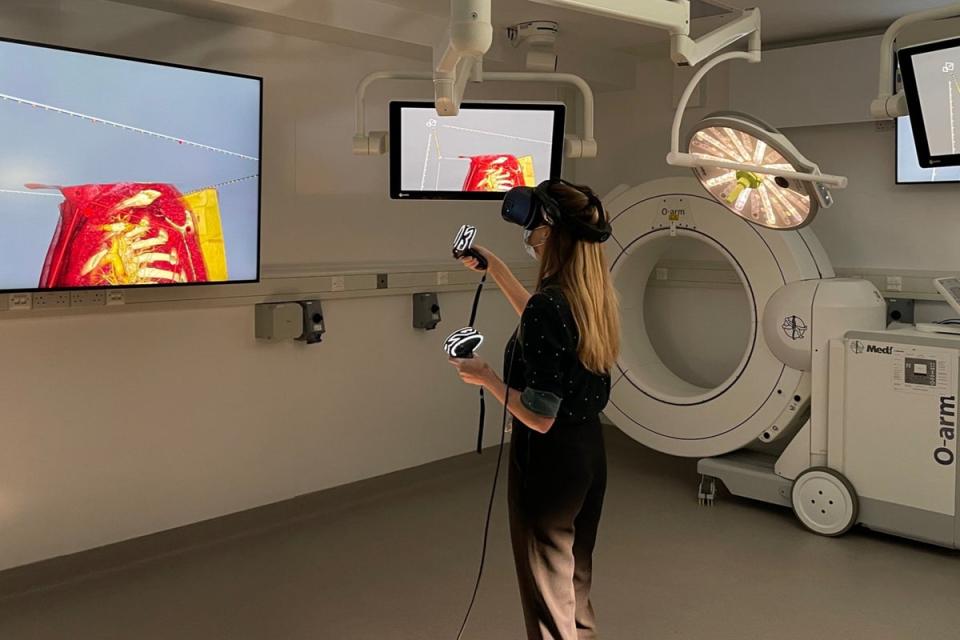
Patients immersed in virtual reality during surgery could require less anaesthetic, according to a new study.
The study saw 34 patients undergoing elective hand surgery at Beth Israel Deaconess Medical Center, in Boston, split into two groups, one given VR headsets and the other one not.
Researchers found that the VR-immersed patients requested significantly lower doses of the sedative propofol – 125.3 mg per hour compared to the average of 750.6 mg per hour during the study.
The VR patients also left the post-anaesthesia recovery unit quicker, spending 65 minutes versus the control group’s 73 minutes.
The research team believes virtual reality helped distract patients from the pain, although they recognised the VR group could have been subject to the placebo effect as they went into the trial thinking that VR would be effective.
The findings, should they be proven in further clinical trials, could help ease the pressure on anaesthetic services in the NHS amid a worsening shortage of anaesthesia professionals, by shortening hospital stays, lowering the risk of complications from excessive dosage, and even saving money on sedatives.
The Royal College of Anaesthetists (RCOA) estimates anaesthetists are involved in the care of two-thirds of hospital patients, from surgeries to maternity to psychiatry. But the current gap of 1,400 anaesthetists means that one million surgical procedures are delayed every year, says the RCOA.
A recent report by the organisation further found that, by 2040, the shortage of anaesthetists will increase to 11,000 unless urgent action is taken across the NHS. The report cited increased demand due to population growth and aging as some of the factors behind this increase.
Retaining anaesthetists is also proving to be difficult, with 50 per cent of those surveyed in the report saying they left the profession or retired due to burnout or excessive workload.
Should the 2040 scenario play out, the RCOA estimates that 8.25 million operations will be unable to take place in the UK due to the lack of anaesthetic staff. This is likely to add considerably to the current record NHS backlog of 6.84 million people waiting for elective care.
While the trial featured a small sample size and will have to be repeated to account for the placebo effect, it is part of a growing body of evidence that suggests virtual reality might indeed help improve patient experience during surgery, in addition to traditional anaesthesia.

 Yahoo Finance
Yahoo Finance 